|
Interrupted Aortic Arch
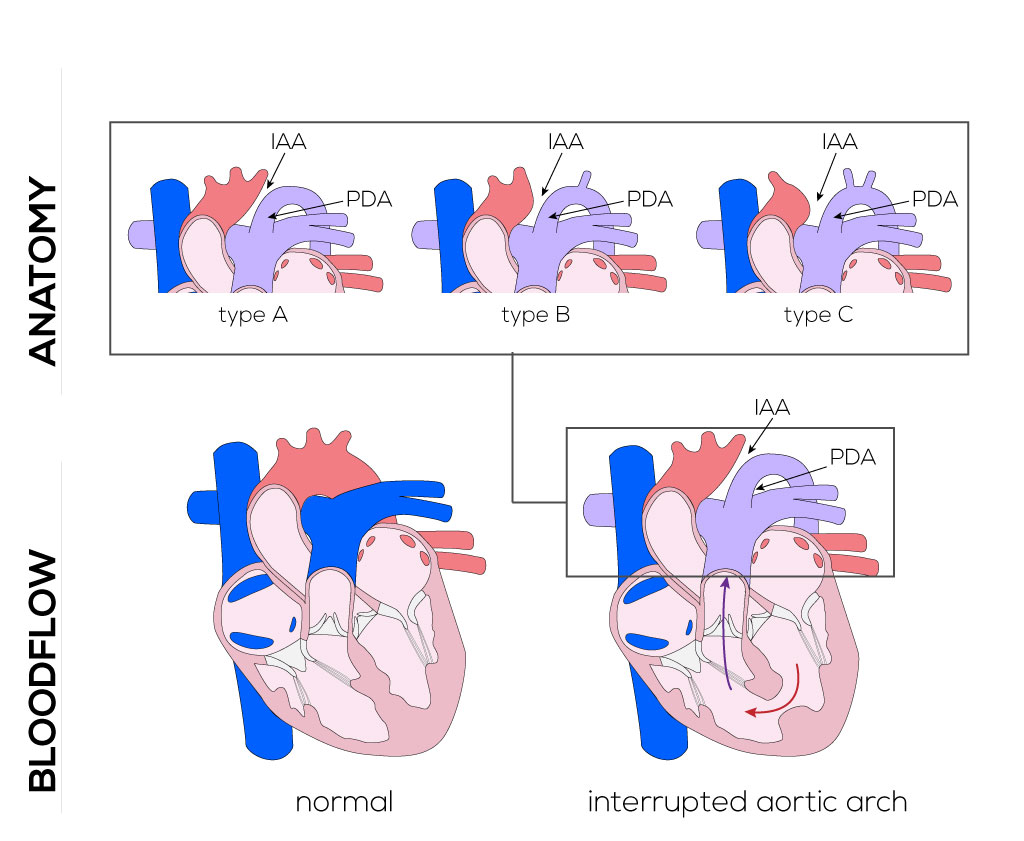
Anatomical description and types
Interrupted aortic arch refers to a lesion involving a loss of continuity between the ascending and descending aorta due to an absence or atresia of an aortic arch. In most cases, this defect is accompanied by a VSD. Other lesions such as aortic stenosis, bicuspid aortic valves, and abnormal subclavian arteries are also common. There are three forms of interrupted aortic arch:
- Type A—an interruption between the left subclavian artery and descending aorta.
- Type B—defect between the left carotid artery and left subclavian artery (most common).
- Type C—interruptions between the innominate and left carotid arteries (least common).
(Click picture to show/hide bloodflows)
Pathophysiology
All three forms of interrupted aortic arch require that there be a patent ductus arteriosus to supply blood to the lower half of the body. Prior to ductal closure, infants will have normally saturated blood perfusing the upper body and deoxygenated blood supplying the lower body. Closure of the ductus a few days after birth prevents blood flow, leading to circulatory collapse and metabolic acidosis, both which threaten survival. The average infant born with an interrupted aortic arch is extremely ill and rarely survives more than a few weeks, typically only a few days.
Therapy
Management of this defect begins with administration of prostaglandin E to maintain a patent ductus arteriosus and blood supply to the lower body. It is recommended that surgical correction take place as soon as metabolic acidosis is controlled. A median sternotomy, cardiopulmonary bypass, and hypothermia are utilized for this procedure. Excision of the ductal tissue and re-anastomosis of the aortic arch are performed to create unobstructed continuity between the parts of the aorta. The anastomosis consists either entirely of native arterial tissue or requires an additional homograft/autograft patch. Any additional defects such as a ventricular septum defect will be repaired contemporarily.
|


