|
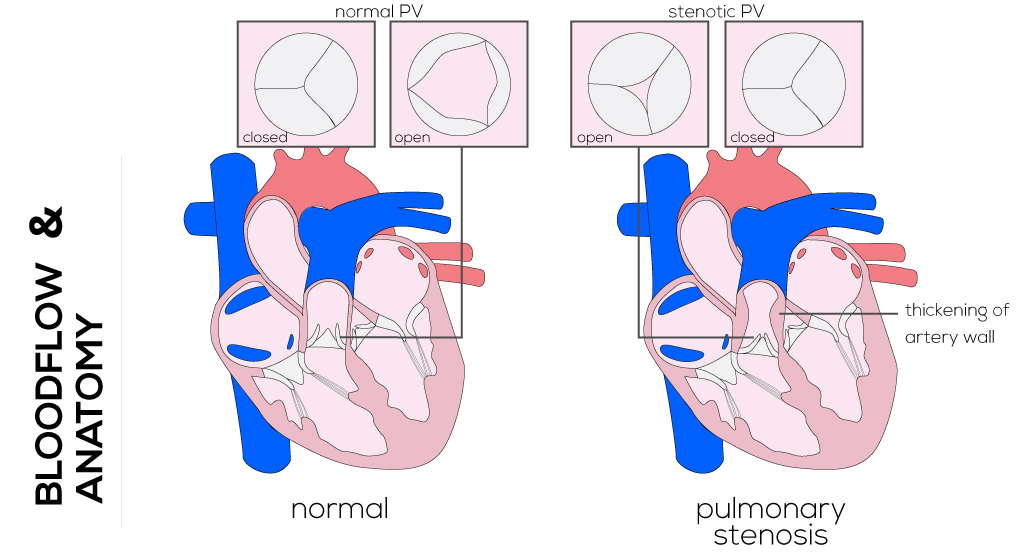
Pulmonary Stenosis
Anatomical description and types
Pulmonary stenosis is characterized by obstruction to outflow from the right ventricle due to a defect in the pulmonary artery, pulmonary valve, or right ventricle itself. It is one of the more common congenital heart defects ranging on a mild to severe spectrum, and is often associated with major primary cardiac anomalies. It can appear in neonates and also beyond the neonatal period.
- Valvar pulmonary stenosis is the most common type of obstruction as a result of either complete absence or fusion of leaflets. In most cases, the valve forms a dome-like structure with a variably sized orifice through which a jet of blood can flow. This pattern of flow results in dilation of the left main pulmonary arteries that receive the jet of blood and, depending on the degree of stenosis, hypertrophy of the right ventricle.
- Subvalvar stenosis, an obstruction within the right ventricle, is less common and often occurs as a result of a VSD that displaces the moderator band. Stenosis of the peripheral pulmonary arteries can be due to any number or combination of lesions, including those that originate in the main pulmonary artery and those found at more locations either unilaterally or bilaterally.
- Supravalvar stenosis describes the situation in which the pulmonary artery lumen above the valve opening is constricted. The obstruction can be located in the main or branch pulmonary arteries.
(Click picture to show/hide bloodflows)
Pathophysiology
Stenosis of the pulmonary outflow tract necessitates an increase in ventricular pressure in order to overcome the obstruction and provide sufficient cardiac output. Over time, the increased pressure leads to hypertrophy and decreased compliance of the right ventricle which, in turn, requires pressure in the right atrium to increase in order to fill the right ventricle. Right-sided heart failure may develop. If the foramen ovale persists and pressure in the right atrium becomes greater than that in the left atrium, blood may begin to shunt right-to-left. Infants born with significant pulmonary stenosis appear cyanotic at birth due to right-to-left shunting and are dependent on a patent ductus arteriosus for adequate blood supply. Because this is a life-threatening condition, it is recommended that balloon dilation be performed to relieve the obstruction as soon as possible. Uncomplicated stenosis of the pulmonary valve is one of the most common congenital heart defects and also the easiest to manage. Infants born with this defect are typically diagnosed at birth on routine physical exam and murmur heard on auscultation. In the absence of septal defects, these children are often asymptomatic.
Therapy
Peripheral pulmonary stenosis is commonly diagnosed by auscultation revealing an ejection murmur heard in all parts of the chest. These obstructions often regress over time and require little or no intervention, depending on the type of the defect as well as the age of the patient. Percutaneous balloon dilation of the valve is the treatment of choice in cases where a significant pressure gradient exists across the stenotic valve in neonates. In neonates, also a surgical valvotomy, angioplasty, and stent insertion must be taken into consideration. Techniques include open and close and with or without cardiopulmonary bypass, depending on the institutional experience. The morphology of the right ventricular outflow tract is an important factor in choosing between balloon and surgical procedure.
The surgical technique begins with a medial sternotomy, mobilization of the thymus, and placement on cardiopulmonary bypass. The patient’s temperature is maintained normothermic and the ductus arteriosus is temporarily occluded. If the valve itself is involved, a longitudinal pulmonary arteriotomy is performed to expose the pulmonary valve, followed by three commissurotomies to achieve maximum orifice without causing insufficiency. In the end, the arteriotomy is closed and the patient can be disconnected from bypass.
In patients with supravalvular stenosis, the pulmonary artery can be widened with a patch of pericardium or prosthetic material. If the stenosis is subvalvular, the obstructing muscle can be reached and excised through the tricuspid valve or directly through an incision into the right ventricular outflow tract.
When pressure gradients are low, most patients do not need any form of treatment and require no restrictions on activity.
|


