|
Heart Block and the Development of the Pacemaker (1957)
An unexpected clinical consequence of the development of open-heart surgery was the discovery of a revolutionary new concept for treatment of complete heart block. Heart block is typically defined as the inability of electrical impulses that begin high in the right atrium to reach the ventricles. Deprived of their normal signal, the ventricles may beat slowly on their own (escape rhythm) or not at all; any prolonged decrease in heart rate that limits a patient's normal activity will typically result in heart failure. At that time, with the only existing treatment for complete block being positive chronotropic drugs or electrodes applied to the surface of the chest, there were no 30-day survivors.
Fortunately, in 1952, Paul Zoll, MD, a cardiologist in Boston, invented the first pacemaker unit, which was a large tabletop external unit with a chest electrode. It was successfully used to resuscitate patients in the hospital, but required the transcutaneous delivery of 50-150 volts, which was incredibly painful for children and typically left scarring blisters.
Complete heart block developed in 10 to 20% of Dr. Lillehei's early patients undergoing closure of ventricular septal defects (e.g., due to induced injury of the heart's conduction system by stitches) and, unfortunately, hospital mortality was 100% in this group of patients. Importantly, early fatality from heart block was completely eliminated with the use of a myocardially placed electrode in combination with an external plug-in electric stimulator [7]. This method of treatment required electrical stimuli of small magnitude (5-10 milliamps and 1-2 volts) and provided very effective control of the heart rate. Such an approach was almost painless but, at that time, it required an AC electrical source, thus limiting the mobility of the patient to the length of the extension cord. It was first used by Dr. Lillehei on a patient in 1957; subsequently an 89% survival rate for patients with prior heart block was reported.
Battery-operated Pacemaker (1958)
The first pacemaker (pulse generator) was a Grass Physiological stimulator borrowed from the University's Physiology Department. This procedure was designed for short-term pacing, with removal of the wires 1-2 weeks after the heart regained a consistent rhythm.
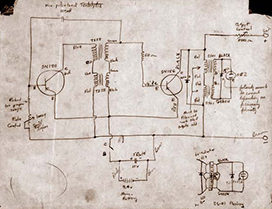
Figure 7. Earl Bakken's original design for the battery-operated pacemaker.
The surgical operating rooms in the 1950s were equipped with EKG and pressure monitoring devices, and the vacuum tubes required frequent monitoring and maintenance to keep them running and calibrated. Hence, the University Hospital subcontracted with a local electric equipment repair company, Medtronic Inc., to perform these maintenance tasks. At that time Medtronic was a two person company - Earl Bakken and his brother-in-law Palmer Hermundslie. Earl was a trained electrical engineer who received his degree from the University of Minnesota. It is reported that, following a disaster during which all electrical power service failed in the University Hospital due to a storm on October 31, 1957, Lillehei eventually asked Earl to design a battery backup for their pacemaker system, to avoid heart block due to power failures. Bakken began this work in 1957, using a circuit modified from a circuit diagram for a transistorized metronome described in a Popular Electronics magazine (Figure 7).
The "battery-powered, wearable pacemaker" was first used clinically in 1958, even though this was somewhat unplanned. Bakken's transistor pulse generator made a miraculous "overnight" transition from pre-clinical animal testing to clinical use. Bakken brought his first prototype to the Surgery Department's research lab, where Dr. Vincent Gott used it on an animal with an imposed heart block and it functioned as planned. That night, Lillehei worked late in the hospital and visited the laboratory where he observed the battery-powered pacemaker performing well; he immediately removed the pacemaker from the animal and brought it to the ICU to use on a patient. The next day, when Bakken arrived back at the hospital, he was overwhelmed to see this device keeping a young child's heart beating.
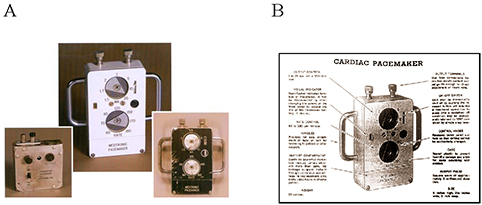
Figure 8. A) The first pacemaker prototype (left), the "Black Box" 5800 external pacemaker (the preliminary test model, right), and the "White Box" 5800 production model (center). B) A page from the Medtronic catalog advertising the 5800 pacemaker.
It was this wearable, battery-powered invention that set the stage for further development in the cardiac pacing industry. For the next decade or so, it would become common practice to put new devices or prototypes (even fully implantable ones) into clinical use immediately, and then iron out the imperfections later based on accumulated clinical experience. This humanitarian practice developed because most of the early patients were close to death, and no other treatments existed [8]. Note that the Food and Drug Administration (FDA) was created by the U.S. government in 1938, but it did not assume the role of regulating medical devices until 1976.
Eventually, Medtronic Inc. became the world's leading manufacturer of cardiac pacemakers beginning with the Model 5800. The first model of the 5800 pacemaker was black, but was quickly changed to white to look cleaner, more sanitary, and "hospital-like" (Figure 8). Between 1959 and 1964, only a few hundred pacemakers were sold due to the reusability of the pacemaker and the short-term post-surgery focus. Orders soared once the pacemaker became implantable and redefined for long-term pacing use.
|


