|
Atrioventricular Septal Defects (AVSD) / Endocardial Cushion Tissue Defects
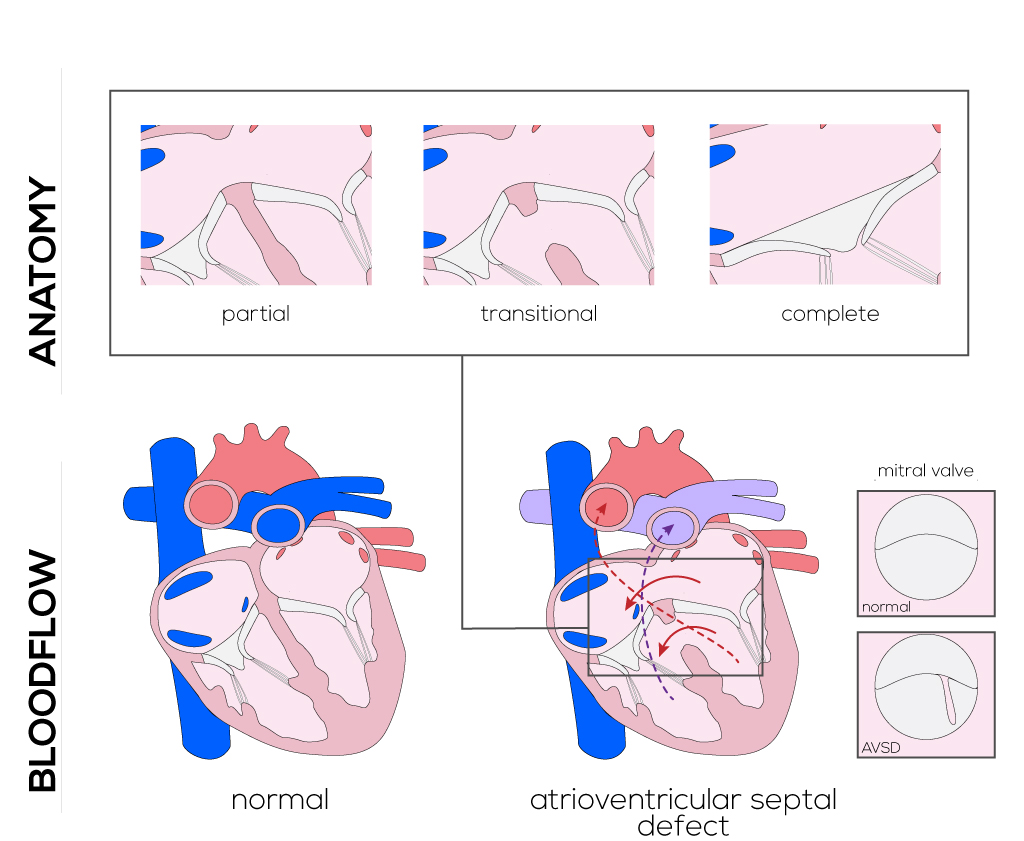
Endocardial cushion defects represent a spectrum of anomalies that arise from an incomplete fusion of the endocardial cushions that participate in formation of the atrioventricular canal, atrial and ventricular septa, and leaflets of the adjacent mitral and tricuspid valves.
Anatomical description and types
Malformations are various and include defects of the mitral valve and tricuspid valve, resulting in a common atrioventricular valve that ranges over the ventricular septum. Defects are primarily due to the total absence of the membranous atrioventricular septum, and are commonly associated with deficiencies in both atrial and ventricular musculature and valves. The atrial septum superior to the plane of the atrioventricular valves can be deficient or absent. The same occurs to the ventricular septum portion to the right inferior of the plane.
AVSDs exist as a continuum with severity ranging from simple, partial defects in the atrial septum to the complete absence of central structures within the heart.
- Partial (incomplete) AV canal defects are characterized by the presence of an ostium primum ASD and clefts in the anterior leaflets of the left atrioventricular valves. There are typically two distinct atrioventricular valves with separate annuli.
- Transitional canal defects consist of two distinct atrioventricular annuli with defects in the atrial and ventricular septa.
- Complete AV canal defects are characterized by a defect in the atrial and ventricular septum leaving a complete, common atrioventricular annulus with an inferior and superior bridging leaflet.
(Click picture to show/hide bloodflows)
Pathophysiology
Partial AV canal defects: A left-to-right shunt at the atrial level results in atrial as well as ventricular dilatation and can lead to pulmonary diseases (see above). Mitral regurgitation and efficiency determine the degree of the defect and influence the left-to-right shunt and left atrial enlargement.
Transitional AV canal defect: The defect behaves more like a partial AVSD. Whereas left-to-right shunting on the atrial level is large, the VSD is usually smaller as in the complete AVSD. Hemodynamics depend on the size of the ventricular shunt and on the manifestation of AV-valve regurgitation.
Complete AV canal defects: Atrioventricular canal defects typically present with atrioventricular valvular regurgitation. Consequently, presented symptoms are similar to those seen from atrial or ventricular septal defects. In addition, an overriding tricuspid valve allows for mixing of pulmonary and systemic venous return. Finally, a large ventricular opening allows for equilibration between the right and left ventricular pressures. A significant left-to-right shunt at atrial and ventricular levels can lead to pulmonary overcirculation and congestive heart failure.
Endocardial cushion defects are commonly secondary diagnoses, and are associated with almost any other type of congenital heart defects except in children with Down syndrome.
Therapy
It is recommended that all types of AVSDs be surgically repaired between 6 and 12 months of age, preferably by age 2 to 3 years to avoid post-operative complications. The specific procedure/repair performed for a patient is dependent on the severity of the defects and presence of associated congenital heart malformities. The principles include closure of the septal defects, interruption of interventricular communication, preservation of a functional conduction system, and ensured competence of two non-stenotic atrioventricular valves. Different methods of cardiopulmonary bypass, hypothermia, circulatory arrest, and cardioplegia are applied according to the situation.
Repair of the septa dividing the atria and ventricles are approached with different patch techniques. Complete common AVSD closure can be accomplished with a single patch made of pericardium or Dacron, or two patches (one for the atrium and another for the ventricle). Further, two separate valves must be reconstructed from the tissue of the common atrioventricular valve; this includes a valvuloplasty and an anuloplasty in order to achieve proper valvular function.
Partial defects require repair of the cleft in the atrioventricular valve utilizing sutures. The primum ASD will be closed by suturing a patch of Dacron or pericardium.
|


