|
Persistent Truncus Arteriosus
Truncus arteriosus is a congenital defect characterized by the presence of a single arterial trunk that originates from the heart.
Anatomical description and types
This proximal ascending vessel is the source of blood supply to both the systemic pulmonary and coronary circulations. The truncus arteriosus defect occurs due to failure in developmental septation of the truncus arteriosus outflow tract. This is caused by the failure of the conotruncal ridges and aortopulmonary septum to develop into the ascending aorta and pulmonary trunk, leaving a single trunk overriding the ventricles and a larger VSD. The pulmonary arteries most often arise from a short vessel branching off the common arterial trunk nearby the valve. Associated defects include deformities and often incompetencies of the truncal valve, an interrupted aortic arch, and coronary artery anomalies. The truncal valve is further abnormal in form, sometimes with two, four, or five valve leaflets rather than the normal three.
Van Praagh has defined four subtypes of persistent truncus arteriosus:
- Type A1 consists of a single arterial trunk originating from a common semilunar valve and immediate bifurcation into ascending aorta and pulmonary artery.
- Type A2 is characterized by both a right and left pulmonary artery that originate from the posterior aspect of the common truncus arteriosus.
- Type A3 describes a single pulmonary artery origin from the truncus (usually the right pulmonary artery).
- Type A4 is also referred to as pseudotruncus and may be better classified as a form of pulmonary atresia with ventriculoseptal defect rather than persistent truncus arteriosus. This defect occurs when the main pulmonary artery is absent and the lungs receive their blood supply via pulmonary collaterals.
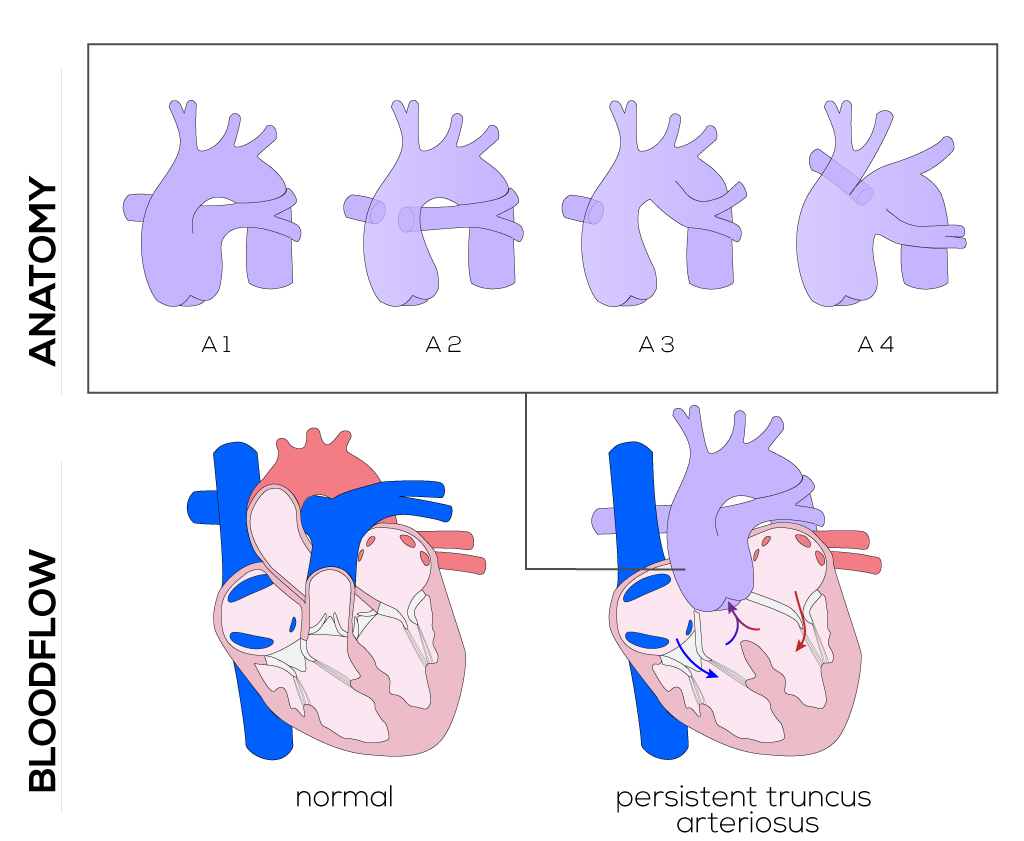
(Click picture to show/hide bloodflows)
Pathophysiology
The result of intracardiac mixing of the systemic and pulmonary venous return is systemic desaturation. In the absence of pulmonary stenosis, the presence of a common arterial trunk supplying both the pulmonary and systemic circulations results in pulmonary arterial pressure equal to that in the truncus itself. As a result, the reduction in pulmonary resistance that occurs after birth is not well tolerated. Increased pulmonary blood flow can lead to flooding of the lungs and early pulmonary vascular obstructive disease. Combined with truncal regurgitation which is present in most cases of persistent truncus arteriosus, many infants develop congestive heart failure within the neonatal period.
Therapy
Surgical correction of these defects is typically performed within days of diagnosis, due to the high prevalence of heart failure and pulmonary vascular obstructive disease which will present early in life. Operative techniques including cannulation, myocardial preservation, and different types of extra-cardiac conduits differ based on institutions and surgeons. Cardiopulmonary bypass, ventricular vent placement, aortic cross-clamping, and cardioplegia are usually applied for this procedure.
The treatment involves closure of the ventricular defect with detachment of the pulmonary arteries from the common trunk, incorporating them into the right ventricle most often with a valved conduit. The conduit material is usually pulmonary/aortic homocraft or bovine jugular vein valved conduit. The VSD is closed with a patch (right ventriculotomy) along with the detachment point of the pulmonary arteries from the common trunk. This procedure preserves all of the anatomical structures such as the coronary arteries. The trunk will function as the aorta and, in case of a stenotic or insufficient truncal valve, surgical correction and replacement of the valve will be attempted.
|


