|
Anomalous Pulmonary Venous Connection
Anatomical description and types
The partial anomalous pulmonary venous return is characterized by at least one but not all pulmonary veins connecting anomalously to the right heart, commonly into the superior vena cava. This defect often occurs together with an ASD and lung abnormalities.
A total anomalous pulmonary connection is specified by drainage of the entire pulmonary venous circulation (all pulmonary veins) into systemic venous vessels which connect to the right atrium. In fact, no pulmonary vein connects to the left atrium.
For the latter pathology, four subtypes have been identified based on the origins of the anomalously draining veins:
- Type I (supracardiac)—occurs when all pulmonary veins return to a common vertical vein, which may drain into a left superior vena cava or brachiocephalic vein.
- Type II (cardiac)—characterized by connection of the pulmonary veins to the common pulmonary vein which drains directly into the heart either via the coronary sinus or right atrium.
- Type III (infradiaphragmatic)—a defect where all pulmonary veins drain into a venous channel that passes through the diaphragm to the portal vein, ductus venosus, or hepatic vein, which then re-enters the heart via the left inferior vena cava.
- Type IV (mixed)—defects that combine two or more of the other types, with any combination of anatomic entry of the pulmonary veins into venous circulation.
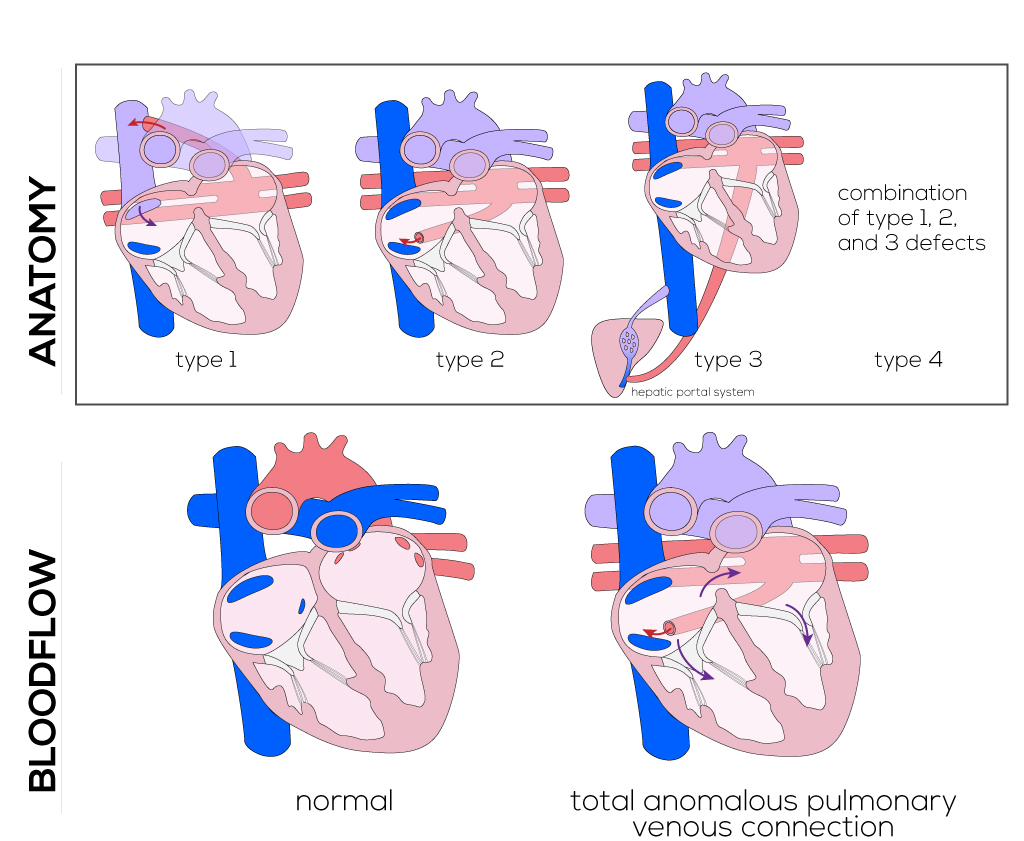
(Click picture to show/hide bloodflows)
Pathophysiology
Patients with partial anomalous pulmonary venous return are usually asymptomatic. The greater the number of pulmonary veins successfully returning to the right side, the more severe are the presenting symptoms.
Children with total anomalous pulmonary connection present with different stages of cyanosis depending on obstruction of pulmonary blood flow and the resulting oxygen saturation. Obstruction of the infradiaphragmatic type is especially severe typically and requires immediate surgery. When obstruction of the pulmonary venous return is significant, the infant will be acutely ill within days of birth. Pulmonary edema will lead to tachypnea and gasping, while mixing of blood supplies leads to cyanosis.
The anomalous pulmonary venous system may have varying levels of obstruction due to compression by adjacent structures, which leads to pulmonary hypertension. Obstruction is typically severe in Type III, as the diaphragm can significantly compress the pulmonary venous structures. Drainage of the entire pulmonary venous system into systemic venous circulation causes mixing of blood, resulting in blood of similar oxygen concentration in all heart chambers. Therefore the patient's arterial oxygen saturation is dependent on the amount of pulmonary blood flow which, in turn, is dependent on pulmonary resistance and obstruction of the pulmonary veins. With large pulmonary blood flow, oxygen saturations can reach the high 80s; in contrast, with limited blood flow, saturations can be much lower and even incompatible with life.
Therapy
Surgical treatment of the presenting anomalies requires accurate anatomical knowledge of all variations in order to place cannulas correctly for cardiopulmonary bypass and open-heart procedures.
The repair of partial anomalous pulmonary veins involves redirection of the veins to the left atrium. Left pulmonary veins that drain superiorly into the innominate vein can be re-anastomosed into the left atrial appendage. Right pulmonary veins that drain into the superior vena cava can be tunneled through the ASD into the left atrium.
The same principles are used to treat total anomalous pulmonary venous return. The pulmonary venous confluence and the left atrium are opened and sutured together. ASDs should be closed with a patch, and anomalous vessels as well as the ductus arteriosus ligated to prevent left-to-right shunts.
|


