|
|
Blood flows throughout the body tissues in blood vessels, via bulk flow (i.e., all constituents
together and in one direction). An extraordinary degree of branching of blood vessels exists within
the human body, which ensures that nearly every cell in the body lies within a short distance from
at least one of the smallest branches of this system: a capillary. Nutrients and metabolic end
products move between the capillary vessels and the surroundings of the cell through the
interstitial fluid by diffusion and mediated transport. Nevertheless, blood flow through all organs
can be considered as passive, and occurs only because arterial pressure is kept higher than venous
pressure via the pumping action of the heart.
In an individual at rest at a given moment, approximately 5% of the total circulating blood is
actually in capillaries. Yet, this volume of blood can be considered to perform the primary
functions of the entire cardiovascular system, specifically the supply of nutrients and removal of
metabolic end products.
The cardiovascular system, is a closed-loop system, such that blood is pumped out of the heart
through one set of vessels (arteries) and then returns to the heart in another (veins). More
specifically, one can consider that there are two closed-loop systems which both originate and
return to the heart: the pulmonary and systemic circulations (see Fig. 1).
The pulmonary circulation is composed of the right heart pump and the lungs. The systemic
circulation includes the left heart pump which supplies blood to the systemic organs. The right and
left heart pumps function in a series arrangement, thus both will circulate an identical volume of
blood in a given minute (cardiac output: liters per minute).
In the systemic circuit, blood is ejected out of the left ventricle via a single large arterythe
aorta. All arteries of the systemic circulation branch from the aorta (this is the largest artery
of the body, with a diameter of 2-3 cm), and divide into progressively smaller vessels. The aorta's
four principal divisions are the ascending aorta (begins at the aortic valve where, close by, the
two coronary artery branches have their origin), arch of the aorta, thoracic aorta, and abdominal
aorta. The smallest of the arteries eventually branch into arterioles. They, in turn, branch into
a extremely large number of the smallest diameter vesselsthe capillaries (with an estimated 10
billion in the average human body). Next blood exits the capillaries and begins its return to the
heart via the venules. Microcirculation is a term coined to collectively describe the flow of blood
through arterioles, capillaries and the venules (Fig. 2).
|
|
|
(click image for larger view)
Figure 1. The major paths of blood flow through pulmonary and systemic circulatory systems. AV = atrioventricular.
|
|
|
Capillaries, which are the smallest and most numerous blood vessels in the human body (ranging
from 5 to 10 micrometers in diameter and numbering around 10 billion) are also the thinnest walled
vessels; an inner diameter of 5 um is just wide enough for an erythrocyte to squeeze through.
Further, it is estimated that there are 25,000 miles of capillaries in an adult, each with an
individual length of about 1 mm. Most capillaries are little more than a single cell layer thick,
consisting of a layer of endothelial cells and a basement membrane. This minimal wall thickness
facilitates the capillary's primary functionto permit the exchange of materials between cells in
tissues and the blood. As mentioned above, small molecules (e.g., O2, CO2, sugars, amino acids, and
water) are relatively free to enter and leave capillaries readily, promoting efficient material
exchange. Nevertheless, the relative permeability of capillaries varies from region to region with
regard to the physical properties of these formed walls. Based on such differences, capillaries are
commonly grouped into two major classes: continuous and fenestrated capillaries
|
|
|
Figure 2. The microcirculation including arterioles, capillaries and venules. The capillaries lie between, or connect, the arterioles and venules.
Capillaries form extensive branching networks that dramatically increase the surface areas available for the rapid exchange of molecules.
A metarteriole is a vessel that emerges from an arteriole and supplies a group of 10 to 100 capillaries. Both the arteriole and the proximal
portion of the metarterioles are surrounded by smooth muscle fibers whose contractions and relaxations regulate blood flow through the capillary bed.
Typically, blood flows intermittently through a capillary bed due to the periodic contractions of the smooth muscles (5-10 times per minute, vasomotion),
which is regulated both locally (metabolically) and by sympathetic control. (Figure modified from Tortora and Grabowski, 2000).
|
|
If a molecule cannot pass between capillary endothelial cells, then it must be transported across
the cell membrane. The mechanisms available for transport across a capillary wall differ for
various substances depending on their molecular sizes and degree of lipid solubility. For example,
certain proteins are selectively transported across endothelial cells by a slow, energy requiring
process known as "transcytosis." In this process, the endothelial cells initially engulf the
proteins in the plasma within capillaries by endocytosis. The molecules are then ferried across the
cells by vesicular transport and released by exocytosis into the interstitial fluid on the other
side. Endothelial cells generally contain large numbers of endocytotic and exocytotic vesicles, and
sometimes these fuse to form continuous vesicular channels across the cell.
The capillaries within the heart normally prevent excessive movement of fluids and molecules
across their walls, but clinical situations have been noted where they may become "leaky." For
example, "capillary leak syndrome," which may be induced following cardiopulmonary bypass, may last
from hours up to days. More specifically, in such cases, the inflammatory response in the vascular
endothelium can disrupt the "gatekeeper" function of capillaries; their increased permeability will
result in myocardial edema.
From capillaries, blood throughout the body then flows into the venous system. It first enters
the venules which then coalesce to form larger vesselsthe veins (see Fig. 2). Then veins from the
various systemic tissues and organs (minus the gas exchange portion of the lungs) unite to produce
two major veins - the inferior vena cava (lower body) and superior vena cava (above the heart). By
way of these two great vessels, blood is returned to the right heart pump, specifically into the
right atrium.
Like capillaries, the walls of the smallest venules are very porous and are the sites where many
phagocytic white blood cells emigrate from the blood into inflamed or infected tissues. Venules and
veins are also richly innervated by sympathetic nerves and smooth muscles within constrict when
these nerves are activated. Thus, increased sympathetic nerve activity is associated with a
decreased venous volume, which results in increased cardiac filling and therefore an increased
cardiac output (via Starling's Law of the Heart).
|
Many veins, especially those in the limbs, also feature abundant valves (which are notably also
found in the cardiac venous system) which are thin folds of the intervessel lining that form
flaplike cusps. The valves project into the vessel lumen and are directed towards the heart
(promoting unidirectional flow of blood). Because blood pressure is normally low in veins, these
valves are important in aiding in venous return by preventing the backflow of blood (which is
especially true in the upright individual). In addition, contractions of skeletal muscles (e.g., in
the legs) also play a role in decreasing the size of the venous reservoir and thus the return of
blood volume to the heart (see Fig. 3).
The pulmonary circulation is composed of a similar circuit. Blood leaves the right ventricle in a
single great vessel, the pulmonary artery (trunk) which, within a short distance (centimeters),
divides into the two main pulmonary arteries, one supplying the right lung and another the left.
Once within the lung proper, the arteries continue to branch down to arterioles and then ultimately
form capillaries. From there, the blood flows into venules, eventually forming four main pulmonary
veins which empty into the left atrium. As blood flows through the lung capillaries, it picks up
oxygen supplied to the lungs by breathing air; hemoglobin within the red blood cells is loaded up
with oxygen (oxygenated blood).
|
|
|
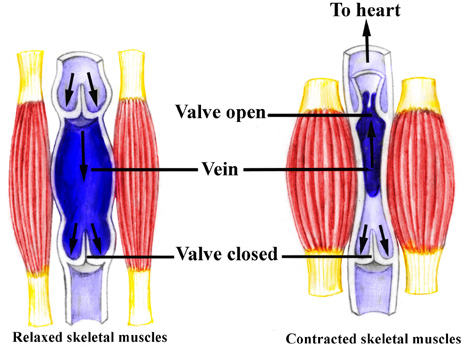
Figure 3. Contractions of the skeletal muscles aid in returning blood to the heartskeletal muscle pump.
While standing at rest, the relaxed vein acts as a reservoir for blood; contractions of limb muscles not
only decrease this reservoir size (venous diameter), but also actively force the return of more blood to
the heart. Note that the resulting increase in blood flow due to the contractions is only towards the
heart due to the valves in the veins.
|
|
|


